

|
Journal Home Contents Preview Next |
Pro Otology
Balkan Journal of Otology & Neuro-Otology, Vol. 3, No 1:9-12 © 2003
All rights reserved. Published by Pro Otology Association
Nystagmus Study after Vestibular Neurotomy:
Contribution of Videonystagmography
R. Meller, E. Ulmer, M. Bruzzo, A. Chays, J. Magnan
Service ORL of Professor Magnan, CHU NORD, Marseille, France.
ABSTRACT
Objective: The investigation of this study researches vestibular features after vestibular neurotomy.
Study design: This is a prospective three-month study.
Setting: Clinic Marseille, France.
Patients: All the 22 tested patients had been treated for an invalidating Meniere disease. All of them had gone vestibular neurotomy. 10 of them - men and 12 - women. In men, the average age was 45.4 years with extreme beetween 15 and 70 years. In women, the average age was 52.5 years with extreme beetween 22 and 61 years.
Interventions: Vestibular neurotomy. Vestibular examination: spontaneous and positional nystagmus, kinetic tests, caloric tests.
Main outcome measures: Precise measurements of the horizontal and vertical components of nystagmus during vestibular testing.
Results: It was found: A spontaneous horizontal nystagmus directed toward the non-operated side in all patients (the intensity of this component decreased with time but was stable after one month); a vertical component in half the cases(always directed upward); positional nystagmus(was frequently found, especially just after surgery, with both horizontal and vertical component involved). Caloric testing did show an unilateral areflexy in each case.
Conclusions: The ideonystagmography may prove the complete section of the vestibular nerve through the total areflexy on the same side of the operation. It gives a precise description of vestibular function after vestibular neurotomy.
Key words: Vestibular neurotomy, Nystagmus, Videonystagmography.
Pro Otology 1: 9-12, 2003
INTRODUCTION
To follow vestibular compensation after vestibular neurotomy, we used videonystagmography. This present several advantages: First, it is seldom being done. After vestibular neurotomy, vertigo complaints usually disappear, and since videonystagmography is a recent tool for the clinician there has been little clinical incentive for in-depth investigation. Second, because the patient population involved is fairly homogeneous with respect to the issue under study. In this study each individual definitely shows a unilateral total peripheral vestibular dysfunction, more or less recent of course.
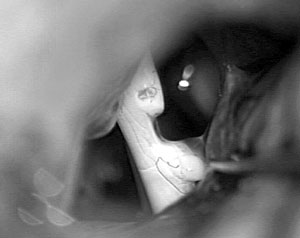
In this prospective study, 22 patients underwent retrosigmoid vestibular neurotomy performed by the same surgeon (FIG. 1) (11).
PATIENTS
The pathology involved was a serious Meniere disease with failure of medical treatment in all 22 cases. Patients were randomly selected, in the sense that during three months, each patient who had undergone a vestibular neurotomy and who was in the department (immediately after neurotomy or for a later control visit) was tested using VNG. 22 patients were tested. 10 of them were men and 12 were women. In men, the average age was 45.4 years with extreme beetween 15 and 70 years. In women, the average age was 52.5 years with extreme beetween 22 and 61 years. The delay beetween operation and testing is given in Table 1.
MEASUREMENTS
|
|
FIG 1. Left vestibular neurotomy using retrosigmoid approach. |
The equipment we used consists of:
- A VNS-VNG system (last model VNG ULMER 99F0203 with torsional analysis, resolution of 1/10 degree and precision of ¼ degree) which allowed to process the signal in real time.
- An electronic chair controlled by a computer and permitting reproducible stimulation
The vestibular examination is done in three stages:
- Spontaneous nystagmus and positional nystagmus. The positions studied are successively dorsal decubitus, right lateral decubitus, left lateral decubitus and anteversion.
- Kinetic tests. During kinetic tests, the patient was seated with his head slightly tilted forward in order to place the lateral semicircular canal in a horizontal position. For each patient, we recorded VVOR (Vestibular Visual Ocular Reflex), then VOR (Visual Ocular Reflex). We studied the gain and the directional preponderance for each patient.
- Caloric tests. The patient is lying on his back, at a 30-degree angle with respect to the horizontal plane. Each ear is irrigated with hot (44 °C) then cold (30 °C) water for 20 seconds. We record the direction and maximal value of the horizontal and vertical components of nystagmus.
RESULTS
VNG permitted in all cases to decompose nystagmus in a horizontal and a vertical component. In all the nystagmus recorded, there was an horizontal component. In almost all the cases, each nystagmus presented also a vertical component.
Spontaneous nystagmus
Horizontal component
Spontaneous nystagmus showed a horizontal component in all cases, even in a patient operated more than 10 years previously (albeit at a very small amplitude). It always beated toward the non-operated side of the neurotomy. We also noticed that the intensity of this component decreases with time. Between 2.5 and 5.0 °/sec right after surgery, it became moderate (1.0 to 2.5 °/sec) after 1 to 3 months, and remained small (less than 1.0°/sec) thereafter.
Vertical component
Spontaneous nystagmus showed a vertical component in half the cases. When present it pointed upward in all cases and its intensity depended on the time lapse since surgery. For patients seen less than three months after surgery, it was between 1.5 and 2.5°/sec in 3/9 of the cases and between 0 and 1 °/sec in 5/9 of the cases. After 3 months it was between 0 and 1 °/sec in 11/13 of the cases, sometimes (2/13) between 1 to 2.5 °/sec but never more than 2.5 °/sec. So, even if the mean intensity of the vertical component seemed to follow the mean intensity of the horizontal component during the time, the correlation of the intensity of the vertical component with the time was clearly less important than the one of the horizontal component.
Positional nystagmus
Horizontal component
Like spontaneous nystagmus, positional horizontal nystagmus when present was always directed toward the non-operated side. Its intensity depended on body position.
Rotation toward the left or the right (along the axis of the body).
Present in 7/22 of patients, it was the more significant component. Most often (5/22) the horizontal component increased when turning toward the operated side; in other cases (2/22), it decreased in intensity when turning toward the opposite side. In either case, the variation was slight (a few degrees per second only). We also noticed that this phenomenon was much more frequent in recently operated patients cases: 5/22 of the cases were seen at 8 days, 1/22 at one month and another 1/22 at three months.
Rotation forward and backward (along transversal axis of the body)
In 30% of cases, we found an increase in the horizontal component not only in lateral decubitus toward the operate side but also in dorsal decubitus.
| Table 1. Delay between vestibular neurotomy and testing. |
|
Vertical component
The rotation forward and backward (along transversal axis of the body) produced the most noticeable effect, with a decrease in the vertical component in the forward position for 22 % of cases.
Kinetic tests
Horizontal component
The VOR gain was found greater than 0.5 in every case. The directional preponderance was, like for spontaneous nystagmus, always toward the non-operated side. Directional preponderance intensity was sometimes equal to, most often greater than the intensity of spontaneous nystagmus.
Like for spontaneous nystagmus, we found a decrease of the intensity of the directional preponderance during time.
Vertical component
In every case, we found less than 0.5 gain and no directional preponderance.
Caloric tests
Horizontal component
When irrigating the operated side, we found no change in spontaneous nystagmus. Vestibular neurotomy did produce an areflexy in each case.
When irrigating the opposite side, we found that hot water produced an intense (>5 °/s) response even a long time after neurotomy. We also found that cold water produced a nystagmus generally directed toward the non-operated side. The intensity of this response is lower than the intensity of the hot water response. In three patients operated less than one month previously, we found a nystagmus directed toward the operated side.
Vertical component
As expected, irrigating the operated side produced no change in spontaneous nystagmus just like for the horizontal component.
For recently operated patients (up to three months), hot-water irrigation of the opposite side resulted in a vertical component pointing downward (68%), upward (22%) or non-existent (4%). The intensity of the response was most often low or moderate (<2.5 °/s). Cold-water irrigation produced a vertical component generally more intense and directed upward in 90% of cases.
DISCUSSION
Spontaneous nystagmus.
Spontaneous nystagmus and postoperative delay
Spontaneous nystagmus is a very useful sign, since we can notice it even with naked eyes in postoperative period. Immediately after a vestibular neurotomy, static and dynamic symptoms can be observed. Curtoys and Halmagyi noticed that the delay of disappearance of spontaneous nystagmus depended on the species (a few hours in the rat, a few days in the monkey or cat and one week in humans) (5). Within one specie, the delay of disappearance of the nystagmus is fairly consistent, which could mean that the vestibular compensation mechanism doesn’t depend on behavior. In the human species, spontaneous nystagmus should disappear in one week (5). However, even one year after vestibular neurotomy, those authors could find spontaneous nystagmus with a very low intensity in patient who had a very good compensation.
Our study goes further. First, and due to the very good sensibility sensitivity the VNG ULMER (2,3,12) we could find an horizontal component of the nystagmus beating toward the controlateral side of the operation in each case even 14 years after neurotomy. The intensity of this nystagmus decreases with time but we did not find any variation after one month. After this period, the intensity stays between 0 and 2 °/s. This nystagmus could persist definitively like a scare as a witness of the intervention. Secondly, we found a vertical component in 50% of the cases even several years after the intervention (one case at 2 years and one case at 14 years with an intensity less than 1°/s).
Vertical nystagmus and central nervous system lesion
Our results show that vertical nystagmus can indeed be present in the absence of any central nervous system impairment. However, in our study this vertical component was absent in half the cases, and when present its intensity was at most half that of the horizontal component. In fact, we were only able to find it thanks to VNG , a powerful tool which can detect very low vertical components. In the past, when physicians detected a “vertical nystagmus” and said it was a sign of central nervous system lesion, they were certainly right because the vertical component they were speaking of was so apparent that they could see it with naked eyes.
Vertical spontaneous nystagmus and central nervous system compensation
When present, the vertical component was always directed upward. We wondered if this sign could be imputed to an ultimate central nervous system compensation. Further studies should verify or disprove this hypothesis.
Positional nystagmus
We observed that horizontal and vertical components vary according to patient’s position. The importance of the variation depends on the delay after surgery. The shorter the delay, the more the variation.
Such a phenomenon could seem to be paradoxical since a vestibular neurotomy causes a “sensorial” and not a “mechanic” impairment of the inner ear as would be a cupulolithiasis for example. However, these findings have been confirmed by several authors (6,8,9,10,13,16).
This study shows that positional nystagmus is a phenomenon that appears with vestibular compensation. Dayal (6) found similar results, but for him vertical positional nystagmus is always a sign of central nervous system impairment. For us, a change in the vertical component during movement could be due to a transitory vestibular compensation state after an acute vestibular lesion. The explanation of this phenomenon is not exactly known, but it could involve a positive or inhibitory action of controlateral otoliths on the vestibular nucleus (16). In addition, Clement found after a flight space an increase in otholitic system sensibility and a longer adaptation of central nervous system to gravity for responses induced by otholits than by semicircular canals (4).
Caloric vertical nystagmus
The appearance of a vertical component with hot or cold water irrigation has been noticed by several authors and led to several interpretations (1,7,14,15).
Contrary to one author, we did not find any difference in the kinetics of the evolution of the parameters of caloric nystagmus between horizontal and vertical component on the non-operated side (1). However, we found that the intensity of vertical nystagmus was less than 50 % that of the horizontal component.
In a few cases, caloric testing did not produce the expected directional inversion of nystagmus. This was observed in cases where the intensity of spontaneous nystagmus was so high, that its direction could not be reversed by a caloric nystagmus directed toward the opposite side.
For horizontal nystagmus, this phenomenon was observed in 3 cases seen less than one month after surgery, when irrigating with cold water. Cold water tended to induce a caloric nystagmus toward the opposite side, but since the neurotomy was recent, spontaneous nystagmus - directed toward the opposite side - was stronger and resulting nystagmus remained on the same side.
For vertical nystagmus, we also found a component directed downward under hot-water irrigation in some cases of recent neurotomy (6 cases seen less than 3 months after surgery).
CONCLUSION
Recent progress in vestibular examination are very important in otology. Nowadays, videonystagmography permits to record in darkness, and very precisely oculomotor reaction. Any nystagmus can be completely described by its component: horizontal, vertical and even rotatory.
This tool is very useful in case of vestibular neurotomy for two main reasons. First, it permits to be sure of the complete section of the vestibular nerve when it shows a total areflexy on the same side of the operation. Moreover, it gives a precise description of vestibular function after vestibular neurotomy and that will certainly help us to follow the evolution of this function with time in these patients and to learn more about vestibular compensation.
REFERENCES
Barber HO, Stoyanoff S. Vertical nystagmus in routine caloric testing. Arch Otolaryngol Head Neck Surg 1986;95:574-80.
Chays A, Ulmer E, Magnan J, et al. La vidéonystagmoscopie: une nouvelle technique d’exporation des troubles de l’équilibre. J F ORL 1995;43:151-3.
Chays A, Ulmer E, Magnan J, et al. Vidéonystagmoscopie. Un nouveau moyen d’exploration des troubles de l’équilibre, Sem Hôp Paris 1994;70:673-7.
Clement G, Darlot C, Petropoulos A, et al. Eye movements and motion perception induced by off-vertical axis rotation (OVAR) at small tilt of angles after spaceflight. Acta Otolaryngol 1995;115:603-9.
Curtoys IS, Halmagyi GM. Vestibular compensation: a rewiew of the oculomotor, neural, and clinical consequences of unilateral vestibular loss. J Vestib Res 1995;5:67-107.
Dayal VS, arkashidy JF, Mai M, et al. Vestibular compensation and nystagmus. Acta Otolaryngol 1984;406:105-9.
Elidan J, Gay I, Lev S. On the vertical caloric nystagmus. J Otolaryngol 1985;14:28-92.
Halmagyi GM, Curtoys IS. A clinical sign of canal paresis. Arch Neurol 1988;45:737-9.
Halmagyi GM, Curtoys IS. Human compensatry slow eye movements in the absence of vestibular function. The vestibular system: Neurophysiologic and clinical research. New York: Raven Press, 1987.
Hamalgyi GM et al. Downbeat nystagmus. A rewiew of 62 cases. Arch neurol 1983;40:777-84.
Magnan J, Bremond G, Chays A, et al. Vestibular neurotomy by retrosigmoid apprroach: technic, indications, and results, Am J Otol 1991;12:101-8.
Magnan J, Chays A, Ulmer E, et al. Videonystagmography: new technology for the functional investigation of vertigo, in: Filipo R, Barbara M, eds. Proceedings of the Third International Symposium on Ménière’s Disease. Amsterdam/New York: Kugler Publications, 1994, 371-4.
Mizuno M, Kudo Y, Yamane M. Upbeat Nystagmus influenced by posture: report of two cases. Auris Nasus Larynx 1990;16:215-21.
Norre ME. Caloric vertical nystagmus: the vertical semicircular canal in caloric testing. J Otolaryngol 1987;16:36-9.
Paige GD. Caloric responses after horizontal canal inactivation. Acta Otolaryyngol 1985;100:321-7.
Toupet M, Pialoux P. Valeur diagnostique du nystagmus vertical dans l’épreuve vestibulaire calorique calibrée bilatérale simultanée. Ann Otol Rhinol Laryngol 1981;98:343-51.
|
Pro Otology |
Journal Home Contents Preview Next |