

|
Journal Home Contents Preview Next |
Pro Otology
Balkan Journal of Otology & Neuro-Otology, Vol. 4, No 1:37—41 © 2004
All rights reserved. Published by Pro Otology Association
Cartilage Palisade Tympanoplasty for Difficult Conditions:
Our Results
C. Uzun, R. Yagiz, Abd. Tas, M. K. Adali, M. Koten, A. R. Karasalihoglu
Otorhinolaryngology Department, Trakya University Faculty of Medicine, Edirne, Turkey
ABSTRACT
Objective: The aim of the present study is to evaluate the use of cartilage palisade tympanoplasty technique for the reconstruction of eardrum in difficult middle ear conditions, such as cholesteatomatous, granulating or adhesive otitis media or simple chronic otitis media with total perforation, and to analyze postoperative results from a group of patients.
Study Design: A retrospective case review.
Setting: Otorhinolaryngology Department, Trakya University Faculty of Medicine, Edirne, Turkey.
Patients: 39 patients with one or more of the following diseases: cholesteatoma, granulating otitis media, diffuse tympanosclerosis, adhesive otitis media and chronic tubagen (simple) otitis media with total or subtotal perforation.
Interventions: We performed cartilage palisade tympanoplasty in 40 ears of 39 patients between July 2001 and December 2003. Thirty-six ears of 35 patients aged 7-57 years were re-evaluated on an average of 12 months postoperatively (range: 3-31 months). The primary preoperative diagnosis was cholesteatoma in 21 ears (58%), granular otitis media in two ears (6%), diffuse tympanosclerosis in 8 ears (22%), adhesive otitis media in four ears (11%) and simple chronic otitis media with total perforation in one ear (3%).
Main Outcome Measures: Postoperative oto-microscopy, pure-tone audiometry (at 250-500-1000-2000-3000-4000-8000 Hz) and speech audiometry.
Results: At the final examination, 5 small perforations and two retractions were seen in contrast to 31 perforations and at least 5 retractions and adhesiveness preoperatively. There was no cholesteatoma recurrence and purulent discharge at the final re-evaluation. The postoperative hearing results were better than the preoperative ones. Preoperative and postoperative mean hearing values were; pure tone average: 48 dB and 35 dB (p=0.0001), and air-bone gap: 31dB and 20 dB (p=0.0001), respectively. Air-bone gap closure within 20 dB or better is achieved in 56% of the ears postoperatively in contrast to 19% preoperatively.
Conclusions: Cartilage palisade tympanoplasty is an effective technique for the reconstruction of the tympanic membrane in difficult middle ear conditions. Good postoperative hearing result may also be achieved after cartilage palisade tympanoplasty.
Key Words: Cartilage palisade tympanoplasty, Chronic otitis media, Tympanic membrane, Perforation, Cholesteatoma, Middle ear surgery
Pro Otology 1:37—41, 2004
INTRODUCTION
Especially in ears with poor middle ear aeration, 80% of the fascia grafts and almost half of the perichondrium grafts atrophy in the following years postoperatively and middle ear atelectasis recurs (1). In order to prevent this and recurrent perforations, cartilage appears to be the key element (2). Postoperative changes can occur after 30 years, but cartilage shrinks only about 30% while fascia and perichondrium shrinks 95%, resulting in blunting of the tympanomeatal niche, atrophic scars with retraction or bulging, recurrent perforations, and drum lateralization (3). As large pieces of cartilage can twist in later years, Heermann and Heermann et al started to use palisades of conchal and tragal cartilage placed parallel to the malleus handle (4,5).The palisade technique is not an easy technique. Several modifications have been developed, such as; Bernal-Sprekelsen’s “three palisades” technique or Neumann’s “roof tiles” technique (6-8). In recent years, use of cartilage and cartilage palisades in the middle ear surgery is increasing. This may be the reason of excellent postoperative results obtained after cartilage palisade tympanoplasty (2-13).
In the present study, Heermann’s original cartilage palisade technique will be discussed in detail, and in this aspect, postoperative results from a group of patients with cartilage palisade tympanoplasty will be evaluated.
MATERIAL AND METHODS
In our department, between July 2001 and December 2003, we performed cartilage palisade tympanoplasty in 40 ears of 39 patients with one or more of those diseases, respectively; cholesteatoma, granulating otitis media, diffuse tympanosclerosis, adhesive otitis media and chronic tubagen (simple) otitis media with total or subtotal perforation. Four patients (four ears) did not show up at the follow-up. The remaining 36 ears of 35 patients were re-evaluated. At the follow-up, oto-microscopy, pure-tone (250-500-1000-2000-3000-4000-8000 Hz) and speech audiometry (speech reception threshold: SRT and speech discrimination score: SDS) were performed. For pure tone average and air-bone gap, an average of thresholds at 500, 1000, 2000 and 3000 Hz (if 3000 Hz was not present, mean of 2000 and 4000 Hz was taken for 3000 Hz) was calculated (14).
When needed (especially in cholesteatoma cases), posterior drilling of the bony annulus (almost in all cases with cholesteatoma), transmeatal atticotomy, modified canal wall-up mastoidectomy (Tos Technique) or canal wall-down mastoidectomy with reconstruction of the posterior canal wall was performed in addition to cartilage palisade tympanoplasty.
When the long process of the incus was defective but with an intact stapes suprastructure, a type II tympanoplasty, when the stapes was absent, a type III tympanoplasty was done.
All patients, including patients with cholesteatoma, were operated on by one of the authors (C.U.) in one stage through retroauricular route.
In all ears, for reconstruction of the eardrum, Heermann’s cartilage palisade technique was performed according to the technique that has been clearly described in detail by Tos and Anderson et al (9,15). The cartilage was most often taken from the concha and rarely from the tragus. The perichondrium was preserved on one side of the cartilage, and thin palisades (approximately 0.5 to 1 mm) were cut by a scalpel blade.
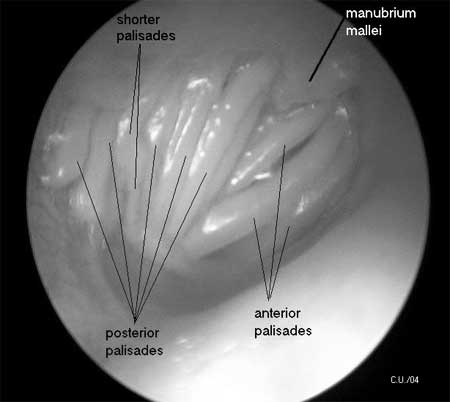
In ears with total perforation, after elevation of the tympanomeatal flap and the fibrous annulus, the first palisade was placed far anterior in the tubal entrance, medial to the bony annulus; the next one was also placed under the bony annulus. The third palisade had close contact with the malleus handle. The next palisades were placed posteriorly to the malleus handle but on the top of the bony annulus. The most posterior palisade was placed with its posterior edge on top of the posterior bony annulus (3-5,15) (FIG. 1).
If perforation is small and inferior part of the drum is intact, the inferior ends of the palisades were usually placed under the remaining eardrum, without contact with the bony annulus.
In ears with ossiculoplasty, the placement of the palisades was adapted to the placement of the interposed ossicle (9). Usually, shorter palisades were placed on the ossicle or between the ossicle and the bony annulus (FIG. 1).
Tos otoscopic clasification was used to subdivide the ears with cholesteatoma in to attic cholesteatoma (attic), with perforation of Shrapnell’s membrane, and tensa cholesteatoma, with perforation of pars tensa (16). Tensa cholesteatoma were further subdivided into sinus cholesteatoma and tensa retraction cholesteatoma. Sinus cholesteatoma is defined as a posterosuperior perforation or retraction (sinus) extending to stapedial niche and tympanic sinus and spreading from here medial to the incus and malleus up towards the attic and aditus. Tensa retraction cholesteatoma (tensa) is defined as a perforation or a retraction of the whole tympanic membrane, including the inferior and anterior segments. The cholesteatoma membrane usually covers the whole tympanic cavity and the tubal orifice and spreads medial to the malleus handle and incus up towards the attic (16).
|
|
FIG 1. Oto-endoscopic appearance of the left ear of a patient 17 months after a successful Combined Heermann And Tos (CHAT) operation made for cholesteatomatous otitis media including adhesiveness, granulation and tympanosclerosis with total tympanic membrane perforation. The perichondrium, which is kept on one side of the cartilage palisades, fuses with the perichondrium of adjacent palisades, whereby the new eardrum is formed, supported by the cartilage palisades. Palisades over the atticotomy are not visible enough because of the fascia cover. Note the shorter palisades over the site of ossiculoplasty. |
RESULTS
Twenty-three of the patients were male and 13 of them were female. The median age at operation was 26.5 years (mean 30.7 years rage: 7-57 years). The postoperative follow-up time was between 3 and 31 months (median: 11 months, mean: 12 months).
The primary preoperative diagnosis was cholesteatoma in 21 ears (58%), granular otitis media in two ears (6%), tympanosclerosis in 8 ears (22%), adhesive otitis media in four ears (11%) and simple chronic otitis media with total eardrum perforation in one ear (3%) (Table 1).
Type I tympanoplasty was performed in 13 ears (36%), Type II in 18 ear (50%) and Type III in 5 ears (14%) (Table 1). Type II tympanoplasty was done with interposition of autologous incus in 16 ears, or sculptured cortical bone or auricular cartilage each in one ear like a “PORP” between stapes and malleus. Type III tympanoplasty was done by either using autologous incus (3 ears) or sculptured cortical bone (one ear) or a hydroxiapetite TORP (one ear) as a columella between the footplate and the malleus handle and/or cartilage palisades.
In 17 ears (47%), tympanoplasty was performed alone. In the remaining 19 ears, an additional surgery was performed: Transmeatal atticotomy in 3 ears, combined Heermann and Tos (CHAT) technique (cartilage palisade tympanoplasty with modified combined approach tympanoplasty, which was introduced by Uzun in 2002) in 14 ears and canal wall-down mastoidectomy with posterior canal wall reconstruction in 2 ears by using auricular cartilage were performed (17,18), (Table 2).
Almost all of the additional surgeries were performed in patients with cholesteatoma (Table 3). Only in one ear with granular otitis media, transmeatal atticotomy was performed in addition to tympanoplasty (Table 3). CHAT technique, which is one of the canal wall-up techniques, could be performed in two-third of the cholesteatoma cases (Table 3).
Almost half of the cholesteatoma cases were attic cholesteatoma (10 ears versus 11 ears with tensa cholesteatoma) (Table 4). Six of the tensa cholesteatoma cases were sinus and 5 were tensa retraction (tensa) cholesteatoma (Table 4).
Preoperative pure tone average was 20 dB or better in only 3% of the ears. After the operation, 22% of the patients obtained a hearing of 20 dB or better and 61% did of 40 dB or better (Table 5). Air-bone gap closure within 10 dB or better was achieved in 28% and 20 dB or better was done in 56% of the ears (Table 5).
The mean preoperative pure tone average level was 48 dB. At the final control, the mean was 35 dB (Paired-Sample T test, p=0.0001). Similarly, the postoperative air bone gap and speech test were significantly better than the preoperative ones (Table 6).
Preoperatively, cholesteatoma was the primary disease in 21 ears. At the follow-up, recurrent cholesteatoma did not develop in any ear (Table 7). Purulent discharge was observed in 12 ears at the time of surgery. However, no purulent discharge was observed at the final re-evaluation. Five perforations (in 3 ears with previous cholesteatoma and 2 ears with adhesive otitis media) were seen at the re-evaluation in contrast to 31 perforations preoperatively, of which almost half (14 ears) were total or subtotal perforations. Four of the five re-perforations were small perforations localized into one quadrant of the eardrum in contrast to localization into 3 or more quadrants preoperatively. In only two ears, postoperative retractions at attic region but clean and stable and with a wide access were observed (Table 7).
| Table 1. Type of tympanoplasty in relation to primary disease. |
|
| Table 2. Type of tympanoplasty in relation to additional surgery. |
|
| Table 3. Additional surgery in relation to primary disease. |
|
| Table 4. Type of cholesteatoma in relation to type of tympanoplasty. |
|
| Table 5. Preoperative and postoperative hearing a mean of one year after the operation (%) |
|
| Table 6. Preoperative and postoperative mean hearing results. |
|
| *Pre- and postoperative speech tests (SRT and SDS) results were available in 28 ears. |
| Table 7. Otoscopic findings before operation and at the final re-evaluation in relation to primary disease. |
|
DISCUSSION
Poor vascularization and Eustachian tube dysfunction may cause graft failures, new retractions and perforations with the potential risk of cholesteatoma formation (8). A high level of mechanical stability of the tympanic membrane is required in order to prevent this (10). Consequently, cartilage slices thicker than 500 micrometer are recommended in chronic tubal dysfunction and adhesive processes (19). In the present study, cartilage slices with a thickness of approximately 0.5-1 mm (500-1000 µm) and perichondrium on one side were used. These cartilage slices did not adversely affect the postoperative hearing results, but significantly reduced the incidence of drum retractions and re-perforations, which are more common in such conditions after reconstruction with fascia (10,12,20).
In tympanoplasty type I, II and III, the hearing result depends on the efficacy of the reconstructed tympanic membrane, the efficacy of the reconstructed ossicular chain and the adequacy of middle ear aeration (21). The palisade technique can provide adequate middle ear aeration. However, for the best hearing result, the palisade technique should be adapted according to the tympanic membrane remnant and reconstruction type (9,10). For example; if some part of the tympanic membrane is intact, ends of the palisades at that part can be placed under the remaining eardrum without contact with bony annulus. In addition, in ears with ossiculoplasty, the placement of the palisades can be adapted to the placement of the interposed ossicle. In the present study, in type II and type III tympanoplasties, short palisades were placed on the ossicle, or between the ossicle and the bony annulus (FIG. 1). These aspects may have influenced the postoperative hearing results. Otherwise, if the palisades have been suspended on the osseous annular rim, the acoustic transfer characteristics of the reconstructed tympanic membrane would have been determined by the stiffness of the cartilage palisade. However, a cartilage island with a regular tympanic membrane surrounding it influences the vibrational characteristics mainly by its mass, as the stiffness of the membrane is determined by the surrounding tympanic membrane remnant (22).
In our study, the graft take rate was 100% although all of the ears were in poor and difficult condition, like cholesteatomatous, granulating or adhesive otitis media. However, five postoperative re-perforations were observed in the early postoperative follow-up. These were small perforations in contrast to total or subtotal perforations preoperatively. The cause of these early re-perforations might be the technical difficulties and faults during packing or unpacking, or due to the learning curve of the surgeon. Because, all of them were observed to occur at the site of a piece of palisade, which might have slid down or up. In contrast, there were no signs or symptoms of recurrent disease, such as purulent discharge or cholesteatoma recurrence. All of them, including the two ears with retraction, were clean and dry, even one year after the surgery. Thus, these patients did not like to have a re-operation for these small perforations. If self-cleaning by migration of keratin debris out of the retraction becomes poor and insufficient, it may lead in long terms to recurrent cholesteatoma (9). Careful long-term observation of such suspected cases is recommended (9). In addition, our rate of closure of the tympanic membrane perforation (84%) was low in contrast to the results reported in the literature (92 to 100%) (2-13), which may be due to the extend and complex disease of our patients. They usually had two or more difficult conditions, such as cholesteatoma, adhesiveness, granulation, tympanosclerosis and total or subtotal perforation, and significant hearing loss more than 40 dB, at the same time of surgery (Tables 1, Tables 5, Tables 7).
In conclusion; cartilage palisade tympanoplasty is an effective technique for the reconstruction of the tympanic membrane in difficult middle ear conditions. Good postoperative hearing results may also be achieved after cartilage palisade tympanoplasty.
REFERENCES
Buckingham RA. Fascia and perichondrium atrophy in tympanoplasty and recurrent middle ear atelectasis. Ann Otol Rhinol Laryngol 1992;101:755-8.
Amedee RC, Mann WJ, Riechelmann H. Cartilage palisade tympanoplasty. Am J Otol 1989;10:447-50.
Heermann J. Autograft tragal and conchal palisade cartilage and perichondrium in tympanomastoid reconstruction. Ear Nose Throat J 1992;71:344-9.
Heermann J. Auricular cartilage palisade tympano-epitympano- antrum- and mastoid plasties. Clin Otolaryngol 1978;3:443-6.
Heermann H, Heermann J, Kopstein E. Fascia and cartilage palisade tympanoplasty: nine years experience. Arch Otolaryngol 1970;91:228-41.
Bernal Sprekelsen M, Lliso MD, Gonzalo JJ. Cartilage palisades in type III tympanoplasty: anatomic and functional long-term results. Otol Neurotol 2003;24:38-42.
Bernal Sprekelsen M, Tomas Barberan M. (Indications, techniques and anatomic results of the tympanoplasty using palisade cartilage). Acta Otorrinolaringol Esp 1997;48:279-86.
Neumann A, Schults-Coulon HJ, Jahnke K. Type III tympanoplasty applying the palisade cartilage technique: a study of 61 cases. Otol Neurotol 2003;24:33-7.
Andersen J, Cayé-Thomasen P, Tos M. Cartilage palisade tympanoplasty in sinus and tensa retraction cholesteatoma. Otol Neurotol 2002;23:825-31.
Uzun C, Cayé-Thomasen P, Andersen J, Tos M. A tympanometric comparison of tympanoplasty with cartilage palisades or fascia after surgery for tensa cholesteatoma in children. Laryngoscope 2003;113:1751-7.
Wiegand H. Knorpelpalisaden und doppelschichtiges Transplantat als Trommelfellersatz. HNO 1978;26:233-6.
Uzun C, Cayé-Thomasen P, Andersen J, Tos M. Eustachian tube patency and function in tympanoplasty with cartilage palisades or fascia after cholesteatoma surgery. Otol Neurotol 2004, in press.
Yu L, Han C, Yu H, Yu D. Auricular cartilage palisade technique for repairing tympanic membrane perforation. Zhonghua Er Bi Yan Hou Ke Za Zhi 2001;36:166-8.
Guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg 1995;113186-7.
Tos M. Manual of middel Ear Surgery, Vol 1. Stuttgart: Thieme Verlag 1995.
Lau T, Tos M. Treatment of sinus cholesteatoma. Long-term results and recurrence rate. Arch Otolaryngol Head Neck Surg 1988;114:1428-34.
Uzun C. Tos technique (modified combined- approach tympanoplasty) and reconstruction with palisade cartilage. Presented at International Interdisciplinary Meeting in Otology and Neuro-Otology (Friendly Meeting), 19-23 May 2002, Stara Zagora, Bulgaria.
Uzun C. Tos technique (modified combined- approach tympanoplasty) and reconstruction with palisade cartilage. Pro Otology (Balkan Journal of Otology
Zahnert T, Hüttenbrink KB, Mürbe D, Bornitz M. Experimental investigations of the use of cartilage in tympanic membrane reconstruction. Am J Otol 2000;21:322-8.
Lau T, Tos M. Tensa retraction cholesteatoma: treatment and long-term results. J Laryngol Otol 1989;103:149-57.
Merchant SN, Ravicz ME, Voss SE, Peake WT, Rosowski JJ. Middle ear mechanics in normal, diseased and reconstructed ears. J Laryngol Otol 1998;112:715-31.
Murbe D, Zahnert T, Bornitz M, Huttenbrink KB. Acoustic properties of different cartilage reconstruction techniques of the tympanic membrane. Laryngoscope 2002;112:1769-76.
|
Pro Otology |
Journal Home Contents Preview Next |