

|
Journal Home Contents Preview Next |
Pro Otology
Balkan Journal of Otology & Neuro-Otology, Vol. 2, No 3:107-108 © 2002
All rights reserved. Published by Pro Otology Association
Audiology in Bulgaria Past, Present and Future
D. Popova, J. Spiridonova
Department of Otorhinolaryngology, University Hospital “Tzaritza Joanna“
Medical University, Sofia, Bulgaria
ABSTRACT
Objective: This report is intended to describe the development of Audiology in Bulgaria today.
Data sources: We have investigated the Bulgarian literature in the last 40 years
Conclusion: We have all modern clinical, audiological investigations, investigate objective the hearing by new borns and little children OAE, BERA, CERA under sedation. They are threshold, suprathreshold and speech audiometry. We make children audiometry and free field audiometry too. We supply the patients with programmable analog and digital hearing aids in the audiological department.Center of Cochlear Implantation is created in the ENT clinic.
Key words: Audiology, Development, Bulgaria.
Pro Otology 3: 107-108, 2002
INTRODUCTION
Audiology in Bulgaria has a 40 years history. After the Second world war, like in other countries, the audiology has rapidly developed.
Audiology and otorhinolaryngology have become sophisticated and highly specialized disciplines. Audiology has increased its ability to study and rehabilitate the hearing impared patients and is becoming from greater and greater importance to the practice of otolaryngology. Its study purposes are related to physiology, pathophysiology of the ear, therapy, rehabilitation and hearing prosthetic.
PAST
In Bulgaria the development of audiology begins in the late 50’s because of growing demands for diagnostic of hearing impared people and for hearing surgery. In 1959, an audiometric cabinet was founded, that was equipped with audiometers “Beoton”. During the first year about 4 – 5000 patients were examined. The next year the use of speech audiometry with monosyllabic test began, as routine practice. After that the other speech tests have been developed (speech threshold tests and speech descrimination tests).
The cortical brainstain evoked potentials were used for the first time in 1971, eight years later, 1978 an auditory evoked responses (ABR) and middle latency auditory evoked potentials were recorded, using surface electrodes. The objective examination of the middle ear was practiced for the first time in1980.
PRESENT
A realisation of the complexity of the ear and its neural pathways and an awareness of many disorders that involve the auditory system make us very much aware of the diagnostic effort that must be made to define the pathology in the given case.
The puretone audiograme and basic word recognition measures remain the key–stone of audiological assesment, defining the degree and pattern of individual hearing loss and documenting auditory communication difficulties. We study and analyse each part of the ear /middle, inner ear, retrocohlear and cortical structures/.
We make a puretone threshold audiometry as a standard behavioral procedure for describing auditory sensitivity. The comparision between air and bone conduction thresholds is important for the otologic diagnosis. After that, when it is necessary we use a free field audiometry, with tonal signal stimulis, usually modulated. This examination is very necessary for the children with cochlear implants and hearihg aids.
When it is necessary to diagnose the sensivity of cochlear function, we use the loudness balance techniques (ABLB) and short increment sensitivity index (SISI) in diagnostic test batteries. These tests are important to distinguish cochlear from retrocochlear pathology, together with tone decay test, immittance and auditory brainstem evoked response techniques.
Threshold audiometry at freguency above 8 khz have a diagnostic and rehabilitative value, and appears to be a valid indication of auditory sensivity.
But a complete understanding of a person’s hearing can be adequated with consideration of how speech is heard under noise conditions. The ability to understand speech is the most important measurement of human auditory function. We are using two basic tests for routinely audiologic examination. The first is a threshold measure for speech understanding. The other speech test is a suprathreshold measure /using monosyllabic words/, to determine the listener’s ability to understand speech under ideal listening conditions. Speech discrimination testing is a part of hearing aid selection procedure. We compare the speech understanding with different hearing aids in quiet and noise and this discrimination ability is one of the factors to determine which ear to fit and the prognosis for successful hearing aids application. The variety of speech stimuli have been used to mapping some patients with cochlear implants.
The acoustic immittance measures are used in our audilogical departement. The clinical application of such measures is the identification and classification of middle ear disorders, function of Eustahiun tube and they are quite effective in the early identifications. The acoustic immittence measure are useful in revealing information on specific disorders of the auditory brainstem and peripheral auditory nervous system. There are quite valuable in the audiologic evaluation of infants, young children and other patients for which behavioral audiometry is not feasible alternative. We are using two major measurement sections - tympanometry and stapedius reflex measure.
|
|
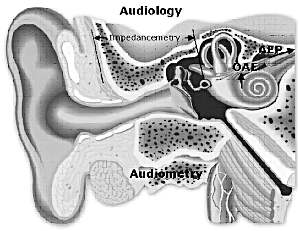
FIG. 1. Methods of audiology. |
Auditory evoked potentials have an essential role in clinical practice of audiology and the other professions.These potentials can be recorded noninvasively with no discomfort to the patient and often with anesthesia. AEP measurement is for us a powerful tool in the diagnosis of audiologic, otologic and neurologic disorders. A hearing loss occurring early in life can have a major impact on speech and language development. It is very important to detect the hearing impairment during the first three years of life, as early as possible and begin intensive education and training with hearing aids or cochlear implants. When we examine the status of hearing, we use the click stimulis to provide information of hearing status in the 500 – 4000 Hz range. The full information of all frequency range we make a threshold at every frequency. The status of speech hearing range is necessary when we prescribe the hearing aids. We use the frequency hearing status when we measure fitting of hearing aids during the time of rehabitation.
Otoacoustic emissions can be used for screening peripheral auditory system disfunction in newborns and infants, separeting the cochlear and neural components of sensoneural hearing loss, monitoring the influence of ototoxic drugs and the intensive sounds of the cochlea. OAE’s can be measured noninvasively and they are valuable addition to clinical audiology.
In our audiological departement when we examine infants, children and adults with a combination of behavioral and electro phisiologic tests. We recommend and determine the need of amplification with hearing aids if it’s necessary. When we prescribe the hearing aids there is a greater reliance on the audiologic factors and motivation factors. We offer for the children to put the binaural hearing aids, when it is possible. In our country we prefer digital hearing aids for young people.
Two years ago we made a cochlear implantation for the first time. We have a centre for cochlear implantation too. Our audiological team are doing evaluation and strong criteria before implantation. After that we make fitting and speech, and hearing rehabilitation. We have now 14 children, prelingualy deaf with MED-EL – Tempo+ , speech processor.
FUTURE
In furure we shall do all to be able to have a new diagnostical and therapeutical possibilities to help the people with hearing impairsments.
REFERENCES
Stamatov GN. Over some problems of hearing impairmence and the rehabilitation oh hearing and speech at children and adults. Plovdiv, 1983.
Shishkov LI. Contemporary methods of hearing examination. Medical Calendar, Sofia, 1969:462.
Shishkov LI. Development of the audiological help in Bulgaria for the period of 1944-1974. ORL 1974;11(3):111-5.
Kehajov A. Guidence of Otoneurology. Sofia: Medicine and Physical Culture, 1982.
Tsenev I. Otorhinolaryngology. Sofia, 1986.
Dimov D, Georgiev G. Ear, nose and throat diseases. Sofia: Publishing house “Knowledgement”, 1998.
Rouev P, Spiridonova J, Dimov P. The possibilities of auditory evoked potentials for early diagnosis of the hearing loss in children. Otorhinolaryngoloia 2001;2:11-8.
Lehnhardt E. Development of CI and the CIC. Hannover: Schnecke, Expo 2000.
|
Pro Otology |
Journal Home Contents Preview Next |