

|
Journal Home Contents Preview Next |
Pro Otology
Balkan Journal of Otology & Neuro-Otology, Vol. 2, No 3:117-120 © 2002
All rights reserved. Published by Pro Otology Association
Incidence of Middle Ear Effusions and Behavior
in Cleft Palate Children
*K. Dzhambazov, Y. Atanassov, *S. Andreeva, *A. Beshkova, L. Epitropova,
R. Simov, Y. Simova
*Clinic of Ear-Nose-Throat Diseases, Medical University, Plovdiv, Bulgaria
Clinic of Craniofacial and Plastic Surgery, Medical University, Plovdiv, Bulgaria
ABSTRACT
Objective: To determine the incidence of middle ear effusions in children with congenital clefts of lips and palate and to develop a concept of the need, type and time of placing ventilation tubes.
Study design: Prospective examination of the middle ear in children with congenital clefts of lips and palate.
Patients: Twenty-eight children with congenital clefts of lips and palate aged between 9 months and 13 years.
Main Outcome Measures: Microotoscopy, audiometry, tympanometry
Interventions: Long-term shunting was performed after paracentesis in 27 children.
Results: Only in one child was found normal hearing and patent Eustachian tubes bilaterally.
Conclusions: Placing long-term ventilation tubes type Paparella (Richards) at the time of surgery for repair of the defect (before the age of 12) has a number of advantages and satisfies contemporary principles of complex therapy of children with congenital clefts of the lips and palate.
Key words: Cleft palate, Otitis media with effusion, Tympanostomy tubes.
Pro Otology 3: 117-120, 2002
|
|
FIG 1. Anatomy of the normal (right) and cleft palate (left).Vertical position of the muscles and their attachment to the bones as well as dysfunction of the tensor veli palatini muscle are the reason for the velopharyngeal insufficiency and serous otitis in patients with palate clefts. |
INTRODUCTION
According to the standards in Europe outlined in the Eurocleft project (1) congenital lip and palate clefts (CLPC) require a multi-disciplinary care involving surgeons, orthodontists, and logopedists. Regarding the high risk of development of serous and later on adhesive otitis inclusion of otorynolaryngologist in the muti-disciplinary team is mandatory in those patients. According to Grant (2) 97% of the children with congenital lip and palate clefts suffer from serous otitis. In another large study (3) including 417 children speech defects were found in 92% and hearing loss due to serous otitis in 80% of the patients. In addition to the operative technique, age at the time of operation and lessons with logopedist the incidence and severity of hearing loss appears of primary importance. Hence, active behavior is recommended in the treatment of this pathology occurring due to dysfunction of the Eustachian tube. It is explained by an aberrant insertion and following dysfunction of the tensor tympani muscle, which can hardly be corrected thoroughly during the palatine surgery (Fig. 1).
Grommet insertion during the surgery for palate repair has been widely accepted recently. This allows the anaesthetic protection to be used and contributes to obtaining better results regarding hearing, speech development and avoiding episodes of recurring otitis media (Fig. 2).
Because of the different opinions about the time of grommet insertion and the necessity of this device in clinically asymptomatic patients we aimed to determine the incidence of the middle ear effusions and develop own conception of behavior in children with this pathology.
MATERIAL AND METHODS
The subjects of the study were 28 children (14 boys and 14 girls) aged between 9 month and 13 years treated in the Clinic of Craniofacial and Plastic surgery of the Medical University in Plovdiv for the period February 2001- February 2002. Due to technical and organization difficulties tympanic membrane and/or hearing status was assessed in 37 out of 55 chidlren subjected to palate surgery. Nine children were excluded from the study because of incomplete examination protocols. Of 28 studied children 6 had bilateral and 12 unilateral lip and palate cleft, while 10 children presented with palate cleft only. All children underwent operative correction of the defect under general anesthesia. Most often in 50% of the cases (14 children), was used technique 1 (uranoplasty after Wardill-Killner-Veau) with transverse dissection of the nasal layer and hamulotomy. These uranoplasties were done in the Clinic before 2000 (Figs. 3,4,5).
Technique 2 (uranoplasty after Wardill-Killner with transverse section of the nasal layer without hamulotomy that was put into practice after 2000) was used in 28.6% and technique 3 including techniques used in other clinics - in 21.4% of the cases. In more than half of the patients (57.1%) the operation was done before the age of 12 months.
Two of the children had case histories of acute otitis media. In the other children the parents did not report of ear problems. Microotoscopy and tympanometry of both ears were performed in all children before the operation. The examination was peformed with impedacemeter Amplaid 720 and in the youngest children assistance of anesthesiologist was required. In children older than 4 years (15 children) hearing was assessed by audiometry.
|
|
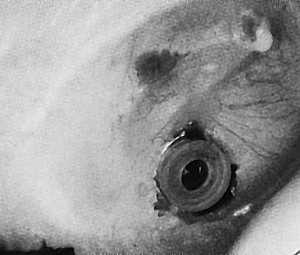
FIG 2. Grommet placed in case of serous otitis. |
RESULTS
Retraction of the tympanic membrane was clearly identified on microtympanoscopy in one of 15 children younger than 4 years. In the other children slight blurring or absence of light reflex was the only symptom observed. There were no other signs of effusion or dysfunction of the middle ear. Notable changes of the tympanic membrane (effusion and initial adhesions) were found at higher incidence in children above the age of 4 in 9 of 13 children (69.2%).
Audiometry was done in 15 children (30 ears). Normal hearing was detected bilaterally in one 3-year-old child and in one more child unilaterally. In all other children (90%) conduction hearing loss varying from 10 to 30 db was present.
Out of 42 ears (21 children) examined by tympanometry only in one child normal type A curve (after Jeger) was found bilaterally and in another child normal impedancemetric curve was found unilaterally. Type B curve was registered in 21 ears (50%) and type C curve (including different subtypes) in 18 ears (35.7%).
Concerning the results after paracentesis long-term grommets type Paparella (Richards) were placed bilaterally in all children (26), excluding the child that presented with normal hearing.
DISCUSSION
Palate clefts represent a typical case of impaired function of the Eustachian tube. Contemporary physiological and morphological studies show that the levator veli palatini muscle does not influence the function of the tube. Of major importance are the hamulus pterygoideus and tensor veli palatini muscle. The superficial and deep parts muscle has antagonistic effects in opening and closing the upper regions and ventilation of the middle ear. Meanwhile in the lower two-thirds of the tube the secretions are drawn toward the epiphrynx. Impairment of this mechanism results in development of serous otitis media effusion in the middle ear without symptoms of inflammation. Serous exutade leaks through intercellular disruptions in the swollen mucous lining of the middle ear and epithelial metaplasia and sticky mucous transudate occur in persisting negative pressure. The middle ear ossicles and tympanic membrane gradually lose elasticity and retract which could result in adhesion to the inner wall of the tympanic cavity with following adhesive otitis and progressive hearing loss. Magnetic resonance imaging of palatine cleft patients with various otological status show anomalies of the tensor veli palatini muscle and hamulus pterygoideus in patients with adhesive otitis (9). These studies raise again the question of the effect of hamulotomy on the middle ear state in surgery of palate clefts.
|

|

|
|
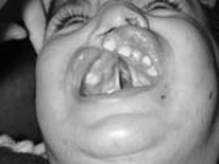
FIG 3, 4, 5. Method of Wardill-Killner-Veau with transverse section of the nasal layer allowing medialisation of the muscles and elongation of the palate. Two arrows on Figure 4 indicate the sectioned muscles. |
||
The otological diagnosis, made by precise audiometry, as well as detailed speech examination are of major importance in the rehabilitation of these children (3).
Hearing loss was established on audiometry in 90% of the children in our study and air conductivity did not exceed 30 db. Although the hearing loss remained within the limits of the socially adequate hearing it could explain the fact that up to 92% of the children with congenital palate clefts have speech problems (3). It is established that, besides the type of the cleft, work of the logopedist and the patient himself, speech rehabilitation depends on the incidence and degree of hearing loss. The cost of the different diagnostic methods for detecting middle ear effusion and the necessity of grommet insertion appear to be of particular interest. Presently the most appropriate age for operative correction of the palate is regarded the age before 12 months. These are the contemporary tendencies in Europe (1). However, the findings of otoscopic examination, even with microscope, are not always univocal and suitable to assess the need of tympanoplasty and the audiometry is not possible. In our study we found clear otoscopic changes mainly in the group of children older than 4 years (69.2%). Changes of the tympanic membrane were evident only in 1 of the children younger than 4 years, which, as we also suggest, offers some difficulties in the assessment of the need of shunting based on otoscopic diagnosis. In this aspect even myringotomy (verifying presence or absence of effusion) could not be used as a reliable criterion for grommet insertion because of the dry ear drums phenomenon that has long been known as pointed by the same authors. As a possible reason for the lack of complete correlation between the findings of all diagnostic methods and the findings of myringotomy is pointed the effect of the general anesthesia on the effusion in the tympanic cavity. The role of the anesthetic agent in changing the pressure in the middle ear and propelling the fluid toward the epipharynx, hypotympanic region or mastoid cells is also taken into consideration.
Fish et al. (10) found a 92% correlation between tympanogram type B (according to Fiellau-Nikolajsen classification) and middle ear effusion established on myringotomy suggesting the best prognostic value of the examination for grommet insertion.
By using impedancemetry we found middle ear effusion in 50% and inadequate middle ear ventilation (type C curve) in 35.7% of the examined ears. In the only case presenting with normal parameters of the middle ear we supposed an intact mechanism of functioning of the Eustachian tube. This could be verified by magnetic resonance imaging, which was unfortunately unavailable to us.
These facts put forth the thesis that up 90% of the patients with congenital palate clefts have impaired function of the Eustachian tube that proceeds after the defect is repaired. Tympanoplasty with long-term shunting is proposed as the only alternative for adequate ventilation of the middle ear to avoid effusion and improve hearing (11,12,13,14).
Studying the hearing in children with congenital clefts Broen et al., 1996 (5) find a correlation between the age of grommets placing and the findings of hearing examination, which allows them to suggest early-age shunting to be preferred. According to us of particular importance is the fact that active accumulation of speech reserves and speech development is most active before the age of 3 (15). Placing long-term Paparella type grommets at the time of surgical repair of the defect (before the age 12) meets these criteria and has the following advantages:
1. Use of general anesthesia.
2. Early therapy of the middle ear effusion or tube dysfunction.
3. Prophylaxis of possible inflammatory complication of the ear.
CONCLUSION
Palate clefts represent a typical example of Eustachian tube dysfunction. Presently impedancemetry is most widely recommended method of diagnosing this pathology. Using this method we succeeded in detecting middle ear effusion in 50% and inadequate ventilation of the middle ear (type C curves) in 35.7% of the ears examined in our study. The active addition of speech resources and speech development is most sufficient before the age of 3. Presently, tympanostomy with placing a long-term grommet is recommended as the method of choice for adequate ventilation of the middle ear in this condition. Placing long-term ventilation tubes type Paparella (Richards) at the time of surgery for repair of the defect (before the age of 12) has a number of advantages and satisfies contemporary principles of complex therapy of children with congenital clefts of the lips and palate.
REFERENCES
Shaw B, Semb G, Nelson P et al. The Eurocleft Project 1966-2000. Standards of Care for Cleft Lip & Palate in Europe. IOS Press, 2000.
Grant HR, Quiney RE, Mercer DM et al. Cleft palate and glue ear. Archives of Diseases in Childhood 1988;63:176-9.
Schonweiler R, Schonweiler B, Schmelzeisen R. Hearing capacity and speech production in 417 children with facial cleft abnormalities. HNO 1994;42(11):691-6.
Greig AVH, Papesch ME, Rowsell AR. Parental perception of grommet insertion in children with cleft palate. The Journal of Laryngology and Otology 1999;113(12):1068-71.
Broen PA, Moller KT, Carlstrom J et al. Comparison of the hearing histories of children with and without cleft palate. Cleft Palate Craniofac J 1996; 33(2):127-33.
Wardill WE.Technique of operation for cleft palate. Br J Surg 1937;25:117.
Veau V. Division palatine. Masson et Cie. Paris, 1931.
Pellerin Ph, Louis Y. Traitement primaire des fentes labio-naso-maxillaires. Dans: Techniques en chirurgie oro-maxillo-faciale. Alain Deboise. Elipses 1993;131-44
Leuwer R, Koch U. Anatomie und Physiologie der Tuba auditiva. HNO 1999;47:514-23.
Fish BM, Banerjee AR, Jennings CR et al. Effect of anaesthetic agents on tympanometry and middle ear effusions. The Journal of Laryngology and Otology 2000;5(114):336-9.
Hubbard TWand coll. Consequences of unremitting middle ear disease in early life. Otological, audiological and developmental findings in children with cleft palate. N Engl J Med 1985;312:1529-34.
Fria T and coll. Conductive hearing loss in infants and young children with cleft palate. J Pediatr 1987;111(1):84-7.
Valtonen H, Qvarnberg Y, Nuutinen J. Tympanostomy in young children with recurrent otitis media. A long-term follow-up study. The Journal of Laryngology and Otology 1999;113(3):207-11.
Dimov P. Chronic serous middle ear otitis. Stara Zagora: Ariel, 1997.
Yules R. Hearing in cleft palate patients. Arch.Otolaryng 91;1970(4):319-23.
|
Pro Otology |
Journal Home Contents Preview Next |