

|
Journal Home Contents Preview Next |
Pro Otology
Balkan Journal of Otology & Neuro-Otology, Vol. 4, No 2-3:122—124 © 2004
All rights reserved. Published by Pro Otology Association
Transnasal Surgical Approach in Choanal Atresia
E. Zenev, J. Tegler, J. Gunnzel, F. Brunner
ENT Clinic, University Hospital Augburg, Germany
ABSTRACT
Objective: Bilateral choanal atresias in newborn are life threatening conditions. Unilateral atresias are more common and their establishment is at later stage of life.
Setting: ENT Clinic, University Hospital Augburg, Germany
Study design: Case report.
Conclusion: This allows introduction of planned and precise surgical correction.
Key words: Choanal atresia, Surgical transnasal approach.
Pro Otology 2-3:122—124, 2004
Introduction
Choanal atresia is defined as uni- or bilateral bone or membranous obturation of choanae, due to intact membrana oronasalis. Data that there are persisting epithelial rests from membrana buccopharyngea are controversial. It is supposed that persisting epithelial cells from early embryological development stages increase in number and lead to a complete obturation of mature choanae. Unilateral atresias are 5 times more frequent than bilateral and 90% of all atresias are bone formatted and 15% - membranous (1).
Associations with other abnormalities are very often. In 15% of the cases there is Charge syndrome (2) which includes: eye coloboma, heart malformations, growth retardation and/or CNS anomalies, genital hypoplasia, malformation of pinna.
Congenital malformations of external and internal nose rearly are not combined with other abnormalities. With advances of perineonatal medicine survival chances of such children rises. Today we meet children with stenoses and tissue obliterations at different sites in the nose as well with patients with cranial stenotic abnormalities of the facial midline (3,4). Choanal atresias represent a typical case of closure of posterior parts of the facial skull.
Respiration of the newborn is mainly nasal. In children with choanal atresia there are frequent changes of apnoic episodes with cyanosis and phases of screaming. Note that ear aspiration is possible only in the time of scream. Swallowing and feeding disturbances due to impaired nasal breathing are common. Some of the suckers adapt quickly and they receive food, but our experience shows that there are more difficulties with oral breathing among premature babies born with multiple malformations.
Unilateral atresia allows anticipating behavior rather than bilateral atresia requires urgent treatment of the neonatal condition (5). When we say immediate treatment we mean insertion of Gudel tube or even intubation. Introduction of tracheostoma should be delayed as much as possible because of the difficulties associated with service and closure of child tracheostoma (3). We should not forget the chance of development of tracheal stenosis. Concerning child’s status it is necessary to perform surgical treatment of choanal atresia as soon as possible.
DIAGNOSIS
Establishment of choanal atresias is based on nasal probing with catheter. If catheter can’t reach approximately 3,5cm diagnosis is positive. We can use also rigid endoscopy and other imaging tools such as profile x-ray examination of the skull with or without introduction of contrast material in nasal cavities. Axial computerized tomography can prove additional cranial and facial malformations (6,7).
TREATMENT
Unilateral choanal atresia can be operated at any proper time and shows clinical signs as unilateral nasal obturation and rhinorhea. Surgical treatment of bilateral atresias should be performed at the very first days or weeks with collaboration with neonatologists. These are recently used surgical techniques (8,9,10):
-Transnasal punction technique – treatment of choice for children with bilateral membranous choanal atresia;
-Transpalatinal approach is useful for the children with bilateral osseus choanal atresia;
-Transseptal approach should be performed in 5 years old children or older. This operation is combined with septoplasty;
-Transnasal microsurgical approach - children with bilateral osseus choanal atresia.
|
|
MATERIAL AND METHODS
We represent a retrospective clinical research with 22 patients treated at Clinicum Ausburg from 1996 till 2003. All of the patients were newborns with congenital osseous choanal atresias. It was met more often in boys than in girls and bilateral versus unilateral lesions were 6:16. All the children were treated surgically with transnasal approach.
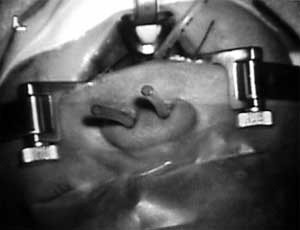
We want to present principles of microsurgical opening of osseus choanal atresia with formation of a lateral mucosal flap for lining and healing the newly created choana (FIG. 1).
To visualize atresia the mouth opener of Digmann and self stabilizing nose speculum in the nose are introduced (FIG. 2). The sickle knife of Draf is used to cut oval mucus flap. After that we deperiostate flap from the underlying osseus obstruction. Then we drill an opening in the choana and cover the opening walls with the flap (FIG. 3). After that a 3,5cm teflon tube (FIG. 4) is intruduced - to support the flap over the opening walls for at least few weeks. Lining of the opening with a mucosal flap on the newly formed choana minimizes the chance of restenosis (11,12,13).

|

|
|
FIG. 3. We drill an opening in the choana and cover the opening walls with the flap. |
|
RESULTS
We didn’t observe complications among presented patients. Surgical procedure is minimally invasive, because of preservation of surrounding tissues and is also well tolerated by the children. It is possible to perform further corrections during widening of the nasal cavities to achieve proper individual positions. There weren’t restenoses in our observations 7 years after the operation.
CONCLUSION
|
|
FIG. 4. Introducing of Teflon tube for support the flap. |
Choanal atresias can be associated with other disorders as pulmonary, heart and myogenic diseases leading to life threatening ventilation disturbances in the newborns. Performing of catheter probing of nasal cavities soon after birth is crucial to on time diagnosis. The newly developed diagnostic tools as rigid edoscopy and imaging techniques are very useful and promising. Tracheostomy should be avoided to prevent further possible laryngotracheal complications. That’s why the aim is operation at earlier days of life. Our experience makes it possible to conclude that the transnasal microsurgical approach is a minimally invasive, elegant and sparing operation.
REFERENCES
Righini ChA, Wroblewski I, Soriano E, Raphael B. Congenital nasal pyriform aperture stenosis: a case report. Rev Laryngol Otol Rhinol (Bord), 2002;123-5.
Maniglia AJ, Goodwin WJ Jr. Congenital choanal atresia. Otolaryngol Clin North Am. 1981 Feb;14(1):167-73.
Brunner FX, Geyer G, Hagen R, Muller J. Klinisch-diagnostische, morpholgische und theraeutische Gesichtpunkte bei Fehlbildungen der äu
Panchal J, Uttchin V;;c. Management of cranoisynotosis. Plast Reconstr Surg. 2003 May; 111 (6):2032-48.
Weintraub AS, Holzmann JR. Neonatal care of infants with head and neck anomalies. Otolaryngol Clin North Am. 2000 Dec;33(6):1171-89.
Jones JE, Young E, Heier L. Congenital bony nasal cavity deformities. Am J Rhinol. 1998 May-Apr;12(2):81-6.
Keller JL, Kacker A. Choanal atresia, CHARGE association and congenital nasal stenosis. Otolaryngol Clin North Am. 2000 Dec;33(6):1343-51.
Zenev, I. Kliniche und Morphologische rhinolaryngologie, Herg. Sofia, 2003.
Osguthorpe JD, Singleton GT, Adkins WY. The surgical approach to bilateral choanal atresia. Analysis of 14 cases. Arch Otolaryngol. 1982 Jun;108(6):366-9.
Sharon-Buller A, Golender J, Savion I, Sela M. Technique for fabrication of splint preventing postsurgical restenosis in choanal atresia. J Prosthet Dent. 2003 Sep;90(3):301-3.
Francis-West PH, Robson L, Evans DJ. Craniofacial development: the tissue and molecular interactions that control development of the head. Adv Anat Embryol Cell BioI. 2003; 169:III-VI,1-138.
Dedo HH. Transnasal mucosal flap rotation technique for repair of posterior choanal atresia. Otolaryngol Head Neck Sirg. 2001 Jun;124-7.
|
Pro Otology |
Journal Home Contents Preview Next |